Treating Endometriosis Pain with Hormones

When is the last time you took a risk? How did it work out?
Today, when I had a procedure done.
I had an IUD pushed through my scar-tissue riddled cervix, with the assistance of an ultrasound machine. An IUD is an IntraUterine Device primarily used for birth control. I don’t need birth control. After removing my second IUD seven years ago, I sank into an unexpected depression while my body relearned how to produce its own progesterone. I worried about what my previous IUDs did to my body and mental health in the 9 years I had one implanted, and I vowed to not get another. How did these hormones change my life in ways that were outside of my control? Shortly after our child was born, my husband had a vasectomy. That was our permanent solution.
Yet, here we are again. What changed my mind?
Endometriosis. It’s changed my life in many ways.
What is Endometriosis?
Endometriosis affects roughly 10% of women of child-bearing age, but awareness of the disease is rare. Why?
Because it’s a women’s issue. It involves periods, which, in 2024, are still “too icky” for most to discuss. Womanhood is deemed shameful, otherwise a natural human process would not be looked at with disdain, causing prevalent ailments to be generally ignored.
When a woman has her period, what many assume to be blood in her underwear or period product isn’t. It’s intrauterine tissue, the walls of the womb shedding in preparation for a potential pregnancy. These womb walls shed and grow again cyclically. It’s natural.
Endometriosis is when intrauterine-like tissue grows outside of the uterus. It can grow on the exterior of the uterus, on the bowels, intestines, ovaries—it’s been found on lungs. Without process to shed this tissue like menstruation, it is left to harden like coagulated blood.
But organs aren’t meant to be hard. They’re meant to expand and contract throughout their common use. If intestines are hard, that translates to pain when food passes through in the process of digestion. If exterior walls of the vagina aren’t elastic, sex will be painful. If the bowels are hardened, eliminating waste will be painful. The list goes on.
Sometimes these lesions can grow in such a way that connects one hardened organ to another. Imagine the potential for pain in that scenario.
On top of that, the body is built to survive. If there is a foreign object, it will act to eliminate it. The body’s attempt to remove this tissue emulates that of menstruation: contracting to push out that tissue. With endometriosis, the tissue has nowhere to go. The contractions intensify. Last time I had a period without hormonal medication (taking the week of sugar pills as prescribed to the average woman avoiding pregnancy), I was laid out on my living room floor writhing in a pain equal to childbirth.
Diagnosis for Endometriosis is Tricky
The lesions are inside the body can evade imaging techniques like ultrasound and MRI. The only way to have a diagnosis with 100% doctor certainty is with a laparoscopy: a surgical procedure where a small incision is made and a thin, lighted tube with a camera called a laparoscope is inserted to examine the organs of the belly.
Laparoscopy is Dangerously Flawed
In my earlier pain days, I fell deep into online and analog resources to learn about the disease. I was desperate for ways to feel better and ways to avoid flare ups.
One of the resources I found, a subreddit, was chock-full of disheartened posts where women put themselves through the physical trauma of a laparoscopy only to be told that they “didn’t have endometriosis.”
This infuriates me. My mother is a physician, I’m not. Yet I know that not seeing something doesn’t mean it isn’t there. I know that perception is flawed, observation is a skill most need to hone, and that not long ago, in a conference full of OB/GYNs that specialize in laparoscopy, the majority only recognized the chocolate-colored lesions that are endometriosis’ hallmark, though it’s been discovered that lesions can be red, black, white, or even appear clear.
Patients who have laparoscopies done by unobservant doctors or those who have not stayed up-to-date are at risk for invalidation and continuing to go untreated.
Endometriosis Diagnosis Alternative to Laparoscopy
Alternatively, OB/GYNs can use prescription effectiveness to determine underlying disease. If hormonal medication alleviates symptoms, you’ve already begun to treat your pain.
Why is Birth Control the Medication Prescribed for Endometriosis?
These pills impede the natural rhythms or fluctuations of the female hormonal flow, instead creating a hormonal steady state. When hormones are not cycling, the pain of menstrual cramps may diminish.
Orbuch, Iris Kerin & Stein, Amy. (2019) Beating Endo: How to Reclaim Your Life from Endometriosis, pp 224
Does Birth Control Heal Endometriosis?
No.
Birth control and other medical treatments treat symptoms only. They do not cure endo; in fact, the endo keeps progressing while you take birth control or other medicines.
Orbuch, Iris Kerin & Stein, Amy. (2019) Beating Endo: How to Reclaim Your Life from Endometriosis, pp 20
Combination Birth Control Pills vs Mini Pill for Endometriosis
I tried the traditional combination birth control pills, that have both estrogen and progesterone, first. To put it bluntly, this medication made me suicidal. The negative mental health outcome was apparent from the offset, but I knew it took several months for hormones to even out.
Six months later, I had been bleeding for three months straight when I asked a gym friend who is an OBGYN doc about it. She suggested I take a a week off and resume.
When I resumed, I experienced that same hopelessness and decided to see my doctor to change my medication. It was then I was prescribed the mini-pill, or Progestin-only Pill (POP).
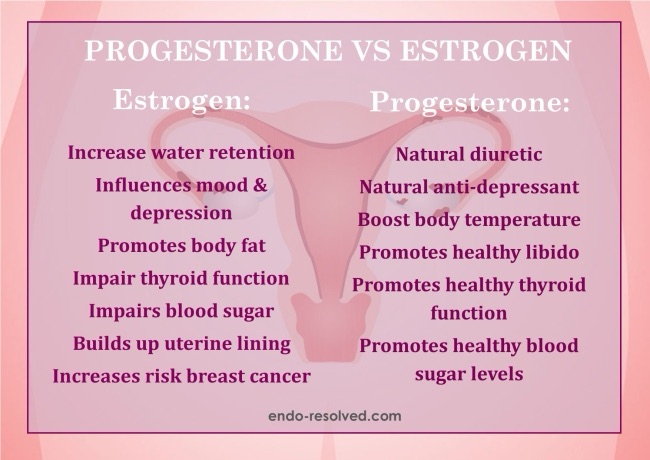
This medication works wonders. Honestly, I’m not quite sure why doctors prescribe combination pills for endometriosis. Endomentriosis is an estrogen-dependent disease, and lesions create their own estrogen. Excess estrogen and progesterone resistance are hallmarks for endometriosis, so why they’re taught to throw more estrogen in the mix is beyond me.
Why IUD?
The progestin was working, so why did I get the implant today? Why go through the pain of sticking something in a hole that’s closed?
The progestin I’m ingesting orally is the same stuff I thought I’d avoid by not having a Mirena IUD. I’m no longer afraid of that hormone with what I know now.
I’ve missed a pill by a few hours and experienced pain for days or even weeks afterward. I’m flawed, there’s no chance I’ll never forget a pill. The benefits of regular hormone release outweighed the cost of expected pain.
I Expected a LOT of Pain.
The last time I had a new IUD inserted was eleven years ago. You can’t recall physical sensations of pain, only the actions you took as you suffered.
In this case, I remembered, all those years ago, having to leave work from the pain. Going home, taking maximum doses of over the counter pain medicines, and breathing rapidly to force myself to sleep by passing out.
How did the risk work out?
If you came here to read daily prompts responses rather than evergreen endometriosis information—wow! You’re still reading! Jokes aside, the procedure went great. We tried the insertion yesterday without success; my doctor didn’t want to force it so today we went to her other office location to try again with ultrasound assistance.
There’s pain, no doubt. But having a chronic pain condition has completely transformed what I deem “unbearable.” This beautiful spring afternoon, I sang on the way home from the doctor’s office. I’ll no longer have to worry about missing a dose.

[…] was struggling through the worst symptoms of Endometriosis when I caved and went the hormone route. Before then, I was reading book after book on my illness and natural pain management to learn to […]